STK11やKEAP1はKRAS変異陽性のときのみICI抵抗性に関与する
非小細胞肺癌でSTK11やKEAP1は免疫チェックポイント阻害剤に耐性を生む変異と言われていたけど、それはKRAS変異の時のみで言えることで、KRAS WT非小細胞肺癌ではSTK11やKEAP1はICI耐性に関連しないようです。米国の主要がん拠点病院のリアルワールドデータの文献です。

STK11 and KEAP1 mutations (STK11MUT and KEAP1MUT) are among the most commonly mutated
genes in lung adenocarcinoma (LUAD). While STK11MUT has been associated with resistance
to PD-(L)1 inhibition in KRAS mutant (KRASMUT) LUAD, its impact on immunotherapy efficacy
in KRAS wild-type (KRASWT) LUAD is currently unknown. Whether KEAP1MUT differentially
impacts outcomes to PD-(L)1 inhibition in KRASMUT and KRASWT LUAD is also unknown.
https://www.jto.org/article/S1556-0864(21)03284-6/pdf
これによると、STK11やKEAP1の変異があり免疫チェックポイント阻害剤による治療を受けたKRAS変異陽性非小細胞肺癌患者ではPFSもOSもHR 2程度と予後が悪い(つまり無増悪生存期間も全生存期間も半分程度になる)というデータがある一方で、このような予後悪化はKRAS野生型非小細胞肺癌では見られなかったとのことです。
これって結構新しい話なのかと思って、過去にSTK11と免疫チェックポイント阻害剤の有効性に関する報告がどのようになっていたのかを辿ってみました。すると、そもそも2018年にSTK11がICI耐性だとか言い始めた頃にすでに「KRAS変異陽性肺癌では」ということになっていたようですね。今回のはそれを再確認しただけの話だったのか…

KRAS is the most common oncogenic driver in lung adenocarcinoma (LUAC). We previously reported that STK11/LKB1 (KL) or TP53 (KP) comutations define distinct subgroups of KRAS -mutant LUAC. Here, we examine the efficacy of PD-1 inhibitors in these subgroups. Objective response rates to PD-1 blockade differed significantly among KL (7.4%), KP (35.7%), and K-only (28.6%) subgroups ( P < 0.001) in the Stand Up To Cancer (SU2C) cohort (174 patients) with KRAS -mutant LUAC and in patients treated with nivolumab in the CheckMate-057 phase III trial (0% vs. 57.1% vs. 18.2%; P = 0.047). In the SU2C cohort, KL LUAC exhibited shorter progression-free ( P < 0.001) and overall ( P = 0.0015) survival compared with KRAS MUT; STK11/LKB1 WT LUAC. Among 924 LUACs, STK11/LKB1 alterations were the only marker significantly associated with PD-L1 negativity in TMBIntermediate/High LUAC. The impact of STK11/LKB1 alterations on clinical outcomes with PD-1/PD-L1 inhibitors extended to PD-L1–positive non–small cell lung cancer. In Kras -mutant murine LUAC models, Stk11/Lkb1 loss promoted PD-1/PD-L1 inhibitor resistance, suggesting a causal role. Our results identify STK11/LKB1 alterations as a major driver of primary resistance to PD-1 blockade in KRAS -mutant LUAC.
Significance: This work identifies STK11/LKB1 alterations as the most prevalent genomic driver of primary resistance to PD-1 axis inhibitors in KRAS -mutant lung adenocarcinoma. Genomic profiling may enhance the predictive utility of PD-L1 expression and tumor mutation burden and facilitate establishment of personalized combination immunotherapy approaches for genomically defined LUAC subsets. Cancer Discov; 8(7); 822–35. ©2018 AACR.
See related commentary by Etxeberria et al., [p. 794][1] .
This article is highlighted in the In This Issue feature, [p. 781][2]
[1]: /lookup/volpage/8/794?iss=7
[2]: /lookup/volpage/8/781?iss=7
https://cancerdiscovery.aacrjournals.org/content/8/7/822
別の報告でも、Fig2を見ると症例数が少ないのですがやはり2018年の時点でSTK11とKRASがダブルで変異を起こしている症例は確かに免疫チェックポイント阻害剤が効いてないようです。ただし、少数例散見されるKRAS野生型症例もSTK11があってもICIが効いているというわけでもないように見えますが…。
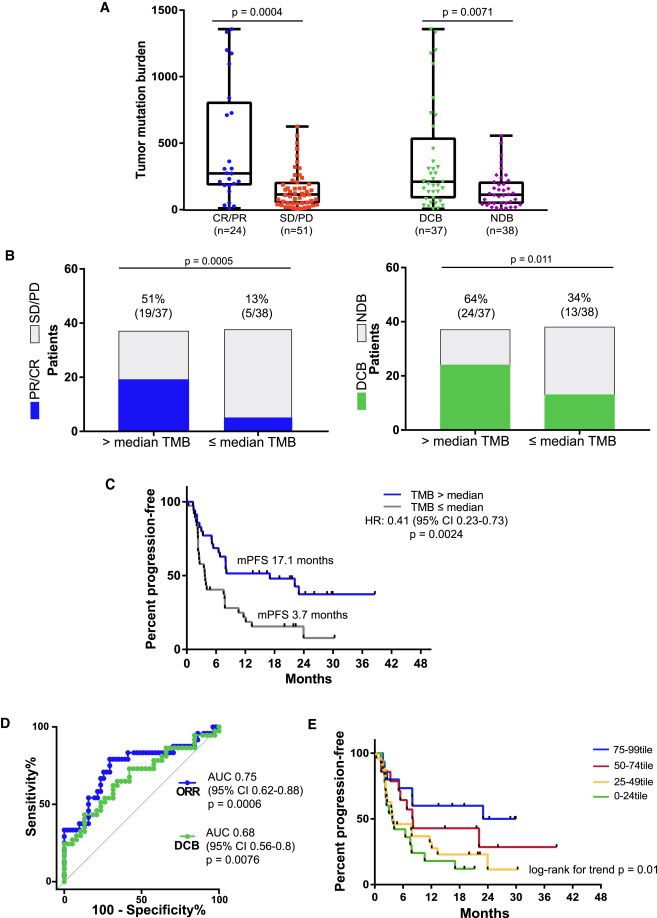
Hellmann et al. examine non-small-cell lung cancers treated with combined PD-1 and
CTLA-4 blockade using whole-exome sequencing and find that high tumor mutation burden
is the strongest feature associated with improved objective response, durable benefit,
and progression-free survival in multivariable analysis.
https://www.cell.com/cancer-cell/fulltext/S1535-6108(18)30123-5
この記事に対するコメント
このページには、まだコメントはありません。
更新日:2021-11-03 閲覧数:730 views.